After a serious case of COVID-19, the long road back to wellness can include many twists and turns.
So, JPS Health Network has assembled a team of experts who get together every other week to serve people who, although they've recovered from the virus, still face its lingering after effects.
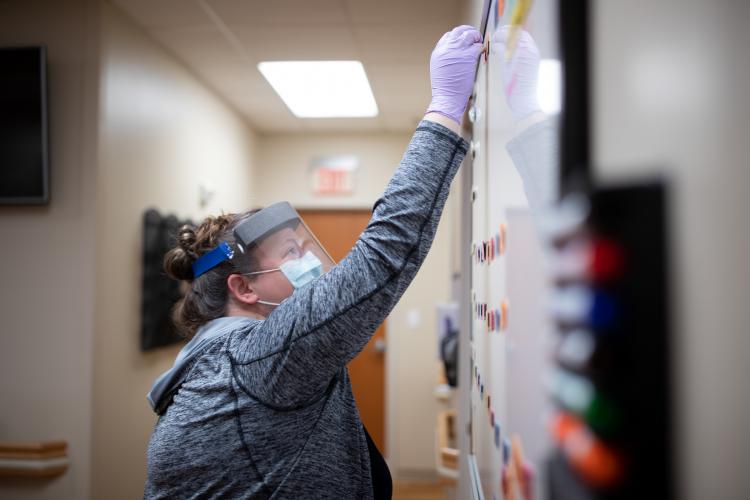
“People recovering from a tough case of COVID have a variety of needs,” said Seme Dewees-Cooper, Practice Manager at the JPS Polytechnic Clinic, which serves as home to the JPS Post COVID Recovery Clinic every other Tuesday. “We have been able to bring together professionals from several different fields who team up to address all of them in one visit.”
At the clinic, instead of going from one appointment to another, likely on several different days, patients only make one visit. They sit in an exam room and, one-by-one, the experts wait their turn to come in to see them. Internal Medicine physicians, Pulmonologists, physical therapists, psychologists, nutrition specialists, and others are on the schedule. Since they're all in the same place, experts can consult with each other on the spot.
“We see lot of people with muscular and skeletal weakness, as well as shortness of breath and cough,” said Internal Medicine physician Dr. Sireeesha Kolachalama. “But we also see a lot of psychological needs. People are suffering from financial setbacks and they’re worried about reinfection. It’s very powerful to be able to address all their issues at once to try to get people back to health. Working together like this for the patients, it’s what makes JPS a special place.”
Pulmonologist Dr. Steven Q. Davis, who organized the Post COVID Recovery Clinic, said bringing different specialists under the same roof is truly the key to giving patients the best care. He said the arrangement gives caregivers the opportunity to discuss patients’ needs in real time, having meaningful discussions instead of trading emails or playing phone tag.
“The pacing really works,” Davis said. “Instead of going to one appointment one day and then another a couple of days later and another a day or two after that, everything can happen in one visit. By the time the patient is done with their visit, there is going to be a plan in place for their care.”
"As long as there are patients who need us, we are going to be here for them."
David Graves, Director of Rehabilitation Services, said physical therapy is an important component of recovery for more reasons than most people might realize. He said he’s glad to be able to get involved in the planning stages of a patient’s recovery so his work can help set the stage for success.
“COVID has a negative effect on the efficiency and pattern of breathing of people who have the disease,” Graves explained, adding that without changes to posture and teaching people how to breathe all over again, they’ll face a much longer and more difficult road to recovery. “A high percentage of COVID patients become ‘chest breathers’ which causes them to work harder to draw in a breath and to not blow the old air out.”
Graves works with recovering COVID patients to train them to breathe from their diaphragm, expelling stale air so they can take in fresh oxygen, improving their ability to heal and rebuild their lost endurance. Then registered dietician Katelin Hatcher visits with patients to talk to them about fueling their body in the proper way to rebuild strength.
“We tell people your body is like a car,” Hatcher said. “If you don’t put gas in it, you’re not going to get anywhere.”
Hatcher said often COVID patients don’t want to eat because of the loss of the senses of taste and smell that are associated with infection. Sometimes, those symptoms linger on long after the person tests negative for the disease. But Hatcher must find ways to get patients to eat the right things even when food of any sort doesn’t seem particularly appetizing.
The specialists who work at the clinic said they’re amazed how naturally it came together when the need for customized care for COVID patients was recognized last spring. Davis said back then no one knew exactly what the long-term needs people would have after battling the disease.
“We’ve been getting a little bit savvier with the things we need to do to treat COVID,” Davis said. “The frustration is that we still don’t know why some people get so much sicker than others. We know what recovery looks like, we know what recovery looks like, we are just are frustrated by our inability to predict who will be hardest hit.”
Currently, the Post COVID-Recovery Clinic sees 8-12 patients a day when it’s open. That number has remained steady over the nine months it has been in operation. The team of caregivers that works there has been rooting for a decrease in hospitalizations and new cases will translate into less demand for long-term care.
“We’ve been hoping to wind down and, at one point, we were hoping to close the clinic by the end of March,” Dewees-Cooper said. “Since then, we’ve decided to keep it open at least through the end of June and, now, it looks like we’ll be here at least through the end of September. As long as there are patients who need us, we’re going to be here for them.”
