Representatives from nursing clinical services have launched a new initiative called the Diabetes Education Program. The program aims to reduce diabetes-related readmissions by providing additional education to patients. The representatives recognized the need for this program due to the lack of knowledge about the disease, identified as the main issue causing readmission. The program was launched in August and has already shown reduced readmissions. Its success lies in the regular follow-up with patients after they have been discharged. During these follow-up calls, patients are asked about their diet, exercise routine, and blood sugar levels and offered improvement recommendations.
The Diabetes Education Program provides a support system to patients and recognizes their progress, which offers positive reinforcement. Many patients call to receive words of encouragement and share their success stories. The program is overseen by two inpatient diabetes educators, Val Smyre, MSN, RN, ONC, RN Certified Diabetes Educator, and Bea Pandit, MSN, RN, CMSRN, RN Certified Diabetes Educator. They see the patients new to diabetes diagnosis, new to insulin, and cardiothoracic patients.
"When I started in February, I was the only full-time educator. I would see patients, provide them all of this education, then a few weeks later I'd see them again,” Smyre said. "I began to see patients repeatedly, so Elisabeth Rodgers, Director Clinical Services, brought this idea over. ‘If we see a patient once, we meet with them again to reinforce the education and provide them with resources. We'll also schedule their follow-up appointments, a meeting with a dietitian, and any outpatient classes provided.'"


JPS serves an underserved population, and there are a few financial barriers that may prevent patients from seeking primary care physicians for follow-up appointments. As a result, patients often resort to using the emergency room as a follow-up appointment, which is not the best use of resources. Since the program's start, JPS has seen only about one to two readmissions per month from newly diagnosed diabetes patients.
"We initially see new diabetes diagnoses and insulin patients on the first day, and we practice the glucometer, syringes, and drawing insulin," Pandit said. "We then follow up the next day and practice with them again to ensure they know what to do before they go home. After the patients are discharged, we like to follow up until they go for their outpatient appointment or outpatient class."
"I always tell my patients to find what motivates them. If you don't find your motivation, it won't work. We're here to guide and help you with the resources. We can answer any questions, but you have to decide if you want to do this or not. You can't change it in a day, but you can get there."
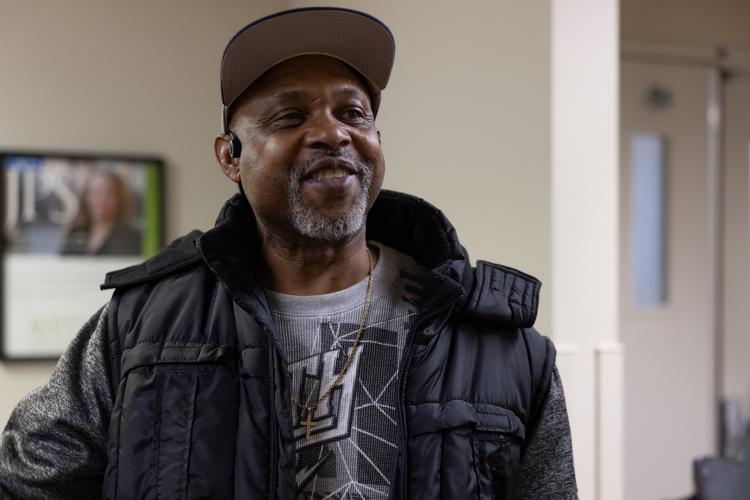
Patient Success Story
Yohann Goodspeed, 56, works as a commercial truck driver. When he was diagnosed with diabetes, he knew that he had to make some lifestyle changes. If he started taking insulin, he wouldn't be able to continue driving, which would have a significant impact on his livelihood.
"If I were to start taking insulin, my medical card would be revoked," Goodspeed said. "You're driving 12 to 14 hours a day, so once you leave the yard, you don't come back until you're finished, and they don't want you taking insulin or having your blood sugar go up and down."
Goodspeed received a pre-diabetic diagnosis a few months prior to his official diagnosis. He said he cut back on a lot, but not the right things. He also didn't take his diagnosis seriously enough. At that time, he was put on oral medication, and he thought he would be okay, but it wasn't enough, and it resulted in his condition worsening. One day, he started to feel really bad and knew something was wrong.
"I had to pull over, and I called my supervisor and explained what was going on. He told me, 'You need to go to the hospital now,'" Goodspeed said. "When I got to the hospital, my blood sugar was almost 400, and I was dehydrated. I was drinking a lot of water, but I wasn't hydrating because my kidneys stopped functioning. It took four bags of saline to flush the creatinine out of my system."
Mr. Goodspeed was presented with the words he didn't want to hear. His provider told him that they were going to discharge him on insulin. Realizing the gravity of the situation, he decided to make the necessary changes in his lifestyle to avoid the need for insulin.
"When I met Mr. Goodspeed, he was a new diagnosis to diabetes," Smyre said. "I went to talk to him, and he said, 'I am not taking insulin. I am four years away from retirement, and I have seen what diabetes does to a person. And realistically, I can't give myself insulin at my job. I really prefer not to take insulin.' I said 'okay,' and I didn't push the issue. I talked to him about what an A1C is, and I showed him a glucose wand. A normal A1C is about an eight, and that's when your blood is moving fast. When it is greater than 10, it's moving slowly – similar to a syrup consistency. I remember showing him, and he said, ‘So you're telling me my blood is like syrup, and it needs to be running?’”
Mr. Goodspeed was motivated to improve his lifestyle after hearing those words. He inquired about his other options and was advised to monitor his blood sugar levels to determine his target range. Additionally, he was encouraged to exercise regularly to help with blood flow. Lastly, he was advised to evaluate his diet and make necessary changes.
"I immediately started walking. That's the main thing I started doing because I wasn't doing that before," Goodspeed said. "Once I started exercising, I started to feel better, and I started to change my diet. I also started to cook for myself, so instead of getting fast food, I'd cook in the mornings. It has also helped me get my blood pressure under control. I feel a lot better now."
During his follow-up appointment, he shared with the diabetes educators that he had been running on the treadmill daily. He even mentioned that his blood sugar had gotten too low due to all the exercise. He told them, "I didn't want to be someone who just talked about making changes; I wanted to prove it to all of you."
"Just listening to him and how he was motivated, empowered, and proud that his blood sugar numbers had decreased stood out to me," Pandit said. "His blood sugar was better than when he was in the hospital, and it felt good because it was more than the results. It was how he felt empowered. We don't see that often because everyone says, 'I don't have the resources' or 'I can't do this.' We hear 'I can't' often, and he proved it was doable. Now we use him as an example when we go see patients."

Goodspeed explains that the education provided by the JPS Health Network Certified Diabetes Educators helped him reach his goal. Once he knew what he needed to do, he was able to make the necessary changes.
"I was taught that diabetes affects your entire body because it's in your blood, and it can damage everything," Goodspeed said. "The biggest thing was understanding how to eat. She explained that when you're buying something from the store, you look at total carbs because that includes sugars, then you'll know how to calculate how many carbs you can eat for one meal, and I eat 65 carbs per meal."
The educators recommend establishing a routine and adhering to it. A diabetes diagnosis is difficult to hear, but with lifestyle changes and motivation, it is manageable.
"I always tell my patients to find what motivates them," Pandit said. "If they have kids, I say, 'think about your kids. Who's going to take care of them? If you don't find your motivation, it won't work. You have to do it. We're here to guide and help you with the resources. We can answer any questions, but you have to decide if you want to do this or not. You can't change it in a day, but you can get there.'"
